Hospital accounts receivable sits at the centre of financial stability in healthcare, yet it is one of the most difficult areas to control consistently. Unlike other industries, hospitals do not deal with a single payer or a simple invoicing cycle. Revenue is split across insurers, government schemes, corporate payers, and patients, each with different rules, timelines, and documentation requirements.
In the UAE and wider GCC, this complexity is amplified by insurance-driven billing, prior authorisations, co-payments, and regulatory oversight. A delay or error at any stage, from patient registration to claim submission or remittance posting, directly impacts cash flow. For finance leaders, this means that strong revenue on paper does not always translate into timely cash in the bank.
Hospital accounts receivable is, therefore, not just an accounting function. It is a core operational discipline that determines liquidity, working capital health, and the organisation’s ability to fund clinical operations without strain.
In this blog, we break down how hospital accounts receivable really works, why collections slow down in healthcare, and what finance leaders can do to stabilise cash flow across complex payer cycles.
TL;DR
- Hospital A/R is an operational outcome, not just a billing metric. Delays almost always originate upstream in registration, documentation, or coding, not at the collection stage.
- Cash flow risk appears long before invoices age. Rising DSO, denial rates, or clean claim slippage are early warnings that revenue will not convert into cash on time.
- Multiple teams shape receivable quality. Treating A/R as a finance-only responsibility ignores the clinical and administrative inputs that determine payment success.
- Denial management drives recovery more than billing volume. Structured follow-up and root-cause analysis recover more revenue than increasing claim throughput.
- Visibility and discipline matter as much as revenue growth. Hospitals with strong A/R controls can fund operations sustainably even in complex, insurance-driven environments.
What Hospital Accounts Receivable Actually Means
Hospital accounts receivable refers to the money owed to a healthcare facility for services already delivered but not yet paid. While this sounds straightforward, the underlying mechanics are significantly more complex than standard trade receivables.
1. It includes multiple payer types
Hospital A/R is made up of insurance claims, government reimbursements, corporate billing, and direct patient balances. Each payer category follows a different payment cycle and dispute process.
2. Payment depends on successful claim adjudication
Revenue is only realised once claims pass insurer checks for eligibility, coding accuracy, coverage limits, and documentation completeness. Any failure here pushes receivables into aging buckets.
3. A/R is deeply embedded in the revenue cycle
Accounts receivable does not start at billing. It begins with patient registration, insurance verification, and clinical documentation. Weaknesses upstream almost always surface later as delayed or denied payments.
4. Multiple teams influence A/R outcomes
Registration staff, clinicians, coders, billing teams, and finance all affect receivable quality. This makes hospital A/R a cross-functional responsibility rather than a finance-only problem.
Understanding these dynamics is critical before attempting to optimise or benchmark receivables performance.
Also Read: Understanding the Procure-to-Pay (P2P) Process
Why Accounts Receivable Matters In Hospitals
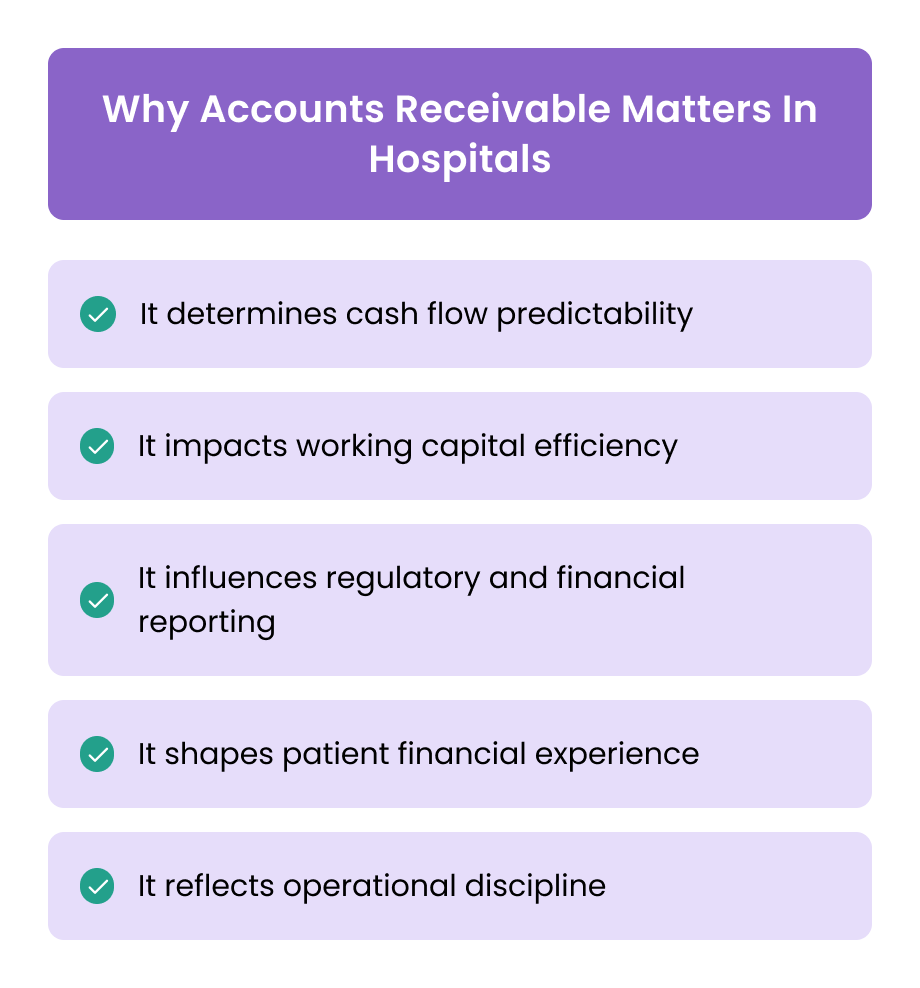
Accounts receivable performance directly affects a hospital’s ability to operate smoothly. Even profitable hospitals can face financial stress if receivables are poorly managed.
1. It determines cash flow predictability
Delayed collections force hospitals to rely on reserves or short-term financing to cover payroll, vendor payments, and clinical supplies.
2. It impacts working capital efficiency
High receivables tie up capital that could otherwise be used for equipment upgrades, staffing, or service expansion.
3. It influences regulatory and financial reporting
Aging receivables, write-offs, and provisions affect financial statements and audit outcomes, especially in regulated healthcare environments.
4. It shapes patient financial experience
Clear, timely billing reduces disputes and improves patient trust. Confusion or delays often result in dissatisfaction and lower collection rates.
5. It reflects operational discipline
Strong A/R metrics usually indicate robust registration, documentation, and billing processes across the hospital.
For finance leaders, accounts receivable is therefore both a financial indicator and an operational health check.
Also Read: Guide to Preparing Financial Statements Efficiently
Core Components Of Hospital Accounts Receivable
Hospital accounts receivable is not a single activity. It is the outcome of several interconnected steps across clinical, administrative, and finance functions. Weakness in any one component usually shows up later as delayed collections or denied claims.
1. Patient Registration And Insurance Verification
Accurate patient details and insurance eligibility checks at registration are the foundation of clean receivables. Errors here, such as incorrect policy numbers or inactive coverage, are among the most common causes of downstream claim rejections.
2. Charge Capture And Medical Coding
Services provided must be captured completely and coded correctly using applicable coding standards. Missed charges or coding inaccuracies directly reduce billable revenue or trigger denials during claim review.
3. Claim Submission To Payers
Claims need to be submitted within payer-specific timelines and formats. Delays or incomplete submissions increase the likelihood of aging receivables and rework.
4. Payer Follow-Up And Denial Management
Not all claims are paid on first submission. Active follow-up with insurers and structured denial management processes are essential to prevent receivables from moving into older aging buckets.
5. Patient Billing And Collections
For co-payments, deductibles, and self-pay balances, clear patient communication and timely billing improve collection rates and reduce write-offs.
6. Remittance Posting And Reconciliation
Payments received from insurers and patients must be accurately posted and reconciled against billed amounts. Errors at this stage distort A/R balances and reporting.
Each of these components contributes to the quality and speed of collections. Effective A/R management requires coordination across all of them, not just billing efficiency.
Also Read: Audit Procedures and Assertions for Accounts Payable
Key Metrics And Benchmarks For Hospital Accounts Receivable
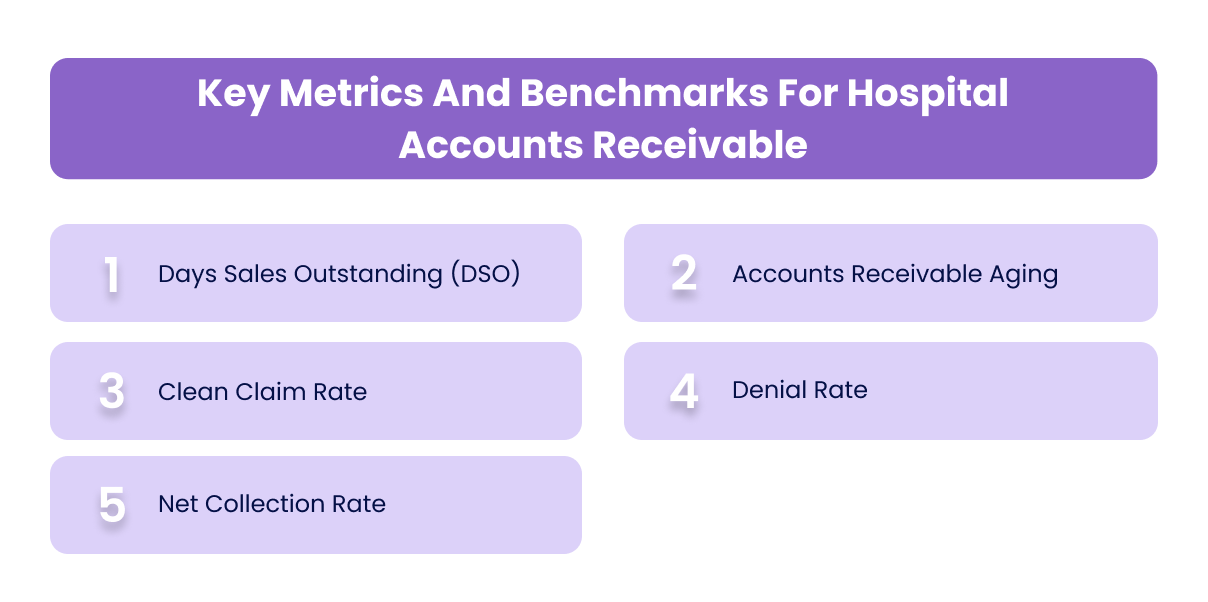
To manage accounts receivable effectively, hospital finance teams rely on a small set of core metrics. These indicators provide early warning signs before cash flow issues become visible.
1. Days Sales Outstanding (DSO)
DSO measures how long it takes, on average, to collect payment after services are rendered. Lower DSO indicates faster collections and healthier cash flow. Persistent increases in DSO often point to claim delays or follow-up gaps.
2. Accounts Receivable Aging
A/R is typically segmented into 0–30, 31–60, 61–90, and 90+ day buckets. A growing proportion of receivables in older buckets signals collection risk and potential write-offs.
3. Clean Claim Rate
This metric tracks the percentage of claims accepted by payers on first submission. Higher clean claim rates reduce rework, speed up payments, and lower administrative costs.
4. Denial Rate
Denial rate reflects the percentage of claims rejected by payers. While some denials are unavoidable, consistently high rates usually indicate systemic issues in documentation, coding, or eligibility verification.
5. Net Collection Rate
Net collection rate measures how much of the collectible revenue is actually collected. It provides a more accurate picture of A/R performance than gross billing figures alone.
These metrics should be reviewed regularly, not just at month end. Early movement in these indicators often precedes larger cash flow challenges.
Also Read: Importance and Steps in Account Reconciliation
Common Causes Of A/R Challenges In Hospitals
Accounts receivable issues in hospitals rarely stem from a single failure. They usually result from small breakdowns across multiple stages of the revenue cycle that compound over time.
1. Incomplete or inaccurate patient information
Errors in demographic details or insurance data at registration often lead to claim rejections or payment delays. These issues are costly because they surface late, when correction requires rework and payer follow-up.
2. Insurance eligibility and authorisation gaps
Services delivered without proper eligibility verification or prior authorisation are frequently denied or partially paid. This pushes receivables into older aging buckets and increases write-offs.
3. Coding and documentation errors
Inconsistent or incorrect clinical documentation affects coding accuracy. Even minor discrepancies can trigger denials or underpayments, slowing collections.
4. Delayed claim submission
Claims submitted late, or in batches without prioritisation, reduce the likelihood of timely payment. Over time, this inflates overall DSO.
5. Weak denial management processes
Denials that are not tracked, categorised, and appealed systematically often remain unresolved. This leads to avoidable revenue leakage.
6. Fragmented billing and accounting systems
When patient billing, claims processing, and accounting operate on separate systems, visibility into receivables becomes limited and reconciliation errors increase.
Understanding these root causes helps finance teams focus improvement efforts where they will have the most impact.
Also Read: Backlog Accounting in UAE: Key Insights and Advantages
Best Practices To Optimise Hospital Accounts Receivable
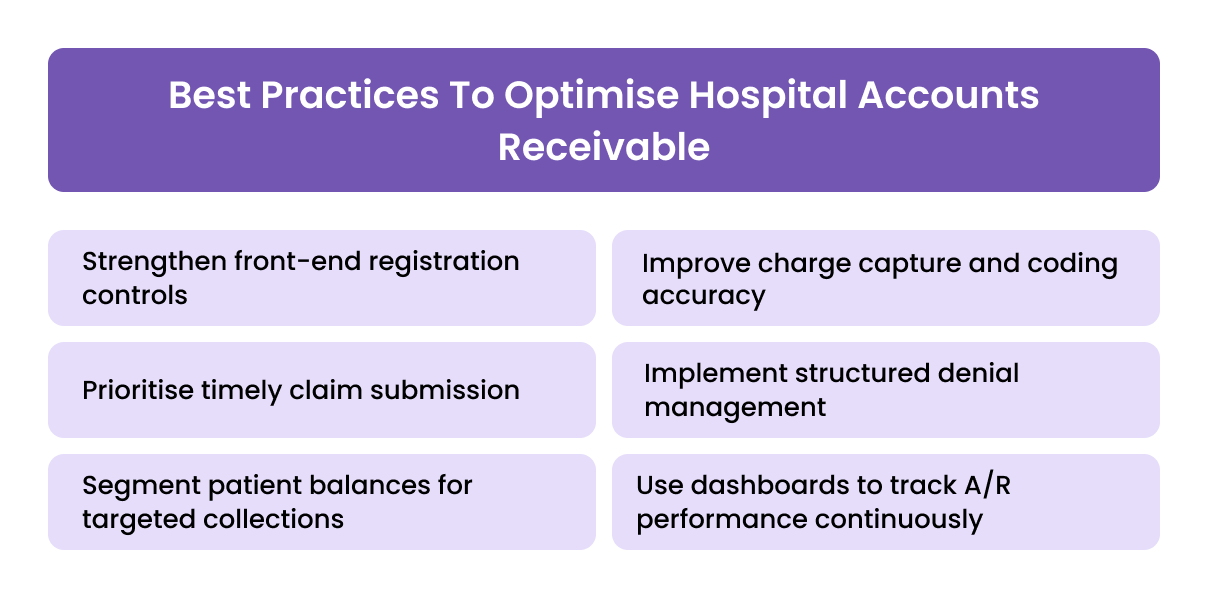
Optimising hospital A/R requires consistency, accountability, and early intervention. The most effective practices focus on preventing issues rather than correcting them later.
1. Strengthen front-end registration controls
Standardising patient intake processes and automating eligibility checks reduce downstream denials and rework.
2. Improve charge capture and coding accuracy
Regular audits and feedback loops between clinical and coding teams help ensure that services are billed completely and correctly.
3. Prioritise timely claim submission
Establishing clear submission timelines and monitoring turnaround times improves payment speed and reduces aging.
4. Implement structured denial management
Categorising denials by root cause and assigning ownership for appeals improves recovery rates and highlights systemic issues.
5. Segment patient balances for targeted collections
Differentiating between insured, self-pay, and corporate balances allows for tailored follow-up strategies and higher collection success.
6. Use dashboards to track A/R performance continuously
Real-time visibility into aging, DSO, and denial trends enables finance teams to intervene before receivables become high risk.
When applied consistently, these practices shorten collection cycles and stabilise hospital cash flow.
Also Read: Understanding Spend Visibility and Business Benefits
Technology And Tools That Support Hospital A/R Management
Given the volume and complexity of hospital billing, manual A/R management quickly becomes unsustainable. Technology plays a critical role in improving accuracy, speed, and visibility across the receivables lifecycle.
1. Hospital Information Systems (HIS) With Integrated Finance Modules
Integrated systems connect patient registration, clinical documentation, billing, and finance. This reduces data handoffs and ensures that receivables are built on accurate clinical and administrative inputs.
2. Rvenue Cycle Management (RCM) Platforms
RCM systems automate claim submission, track payer responses, and manage follow-ups. They help standardise workflows and reduce dependency on manual tracking.
3. Claim Scrubbing And Coding Validation Tools
Automated checks identify coding errors and missing information before claims are submitted. This improves clean claim rates and shortens payment cycles.
4. Denial Management Software
These tools categorise denials by reason, payer, and department. Over time, they provide insights into recurring issues and support targeted process improvements.
5. Electronic Remittance Advice (ERA) And Auto-Posting
Automated remittance posting reduces reconciliation errors and speeds up the transition from payment receipt to accurate A/R reporting.
6. A/R Analytics And Dashboards
Real-time dashboards give finance teams visibility into DSO, aging buckets, denial trends, and payer performance, enabling earlier intervention.
Technology does not replace strong processes, but without it, scaling and sustaining A/R performance is extremely difficult.
Regulatory And Compliance Considerations In UAE And GCC Healthcare A/R
Hospital A/R management in the UAE and GCC operates within a regulated environment that directly affects billing, collections, and reporting.
1. Insurance And Payer Regulations
Hospitals must comply with insurer-specific billing rules, documentation standards, and submission timelines. Non-compliance often results in claim rejections or delayed payments.
2. VAT Treatment Of Healthcare Services
While many healthcare services are zero-rated or exempt, errors in VAT treatment can complicate billing and reconciliation. Finance teams must ensure correct classification and documentation.
3. Patient Data Protection And Confidentiality
Financial data in healthcare is closely linked to patient information. Compliance with data protection requirements is essential when managing billing systems and A/R data.
4. Audit And Record-Keeping Requirements
Hospitals are required to maintain detailed billing and payment records for regulatory reviews and audits. Poor A/R documentation increases compliance risk.
5. Price Transparency And Billing Accuracy
Increasing regulatory focus on transparent pricing places greater emphasis on accurate billing and clear patient communication.

Finance teams must factor these requirements into A/R processes to avoid regulatory risk while maintaining efficient collections.
How Alaan Supports Healthcare Finance Teams Beyond Revenue Cycle Systems
Hospital revenue cycle platforms focus on billing, claims, and collections. That work is essential, but it only addresses one side of working capital. While receivables move through complex payer cycles, hospitals still need tight control over day-to-day operational spend to protect liquidity.
At Alaan, we support healthcare finance teams by strengthening visibility and discipline on the spend side of the equation. This matters because delayed receivables often coincide with ongoing expenses such as medical supplies, vendor payments, facilities costs, and staff-related spend that cannot wait for insurance reimbursements.
Alaan helps hospitals:
- Maintain real-time visibility into operational spend while receivables are pending, allowing finance teams to manage cash more confidently during long payer cycles.
- Control approvals and payments centrally, reducing leakage and unplanned outflows at a time when cash inflows are delayed.
- Improve working capital discipline by ensuring expenses, approvals, and accounting entries are captured accurately and on time.
- Align spend control with financial reporting, so finance teams are not managing receivables in isolation from outgoing cash commitments.
By bringing structure and visibility to everyday spending, Alaan helps healthcare organisations stay financially stable while revenue cycle systems handle the complexity of billing and collections. This balance becomes increasingly important in environments where payer timelines are unpredictable and margins are sensitive.
Conclusion
Hospital accounts receivable is not simply a billing outcome. It is the financial reflection of how well clinical, administrative, and finance teams work together across the revenue cycle. When A/R processes are weak, even high patient volumes and strong service demand fail to translate into stable cash flow.
For healthcare finance leaders, improving accounts receivable requires a shift in focus. The priority moves from chasing aged balances to preventing delays through better registration controls, cleaner claims, disciplined follow-up, and real-time visibility into performance metrics. Hospitals that treat A/R as an operational discipline rather than a back-office function are better positioned to maintain liquidity, meet regulatory expectations, and fund clinical excellence.
In a sector where margins are sensitive and working capital matters, strong hospital accounts receivable management is a prerequisite for sustainable operations.
At Alaan, we work with healthcare finance teams to improve visibility into day-to-day operational spend that directly affects working capital. While clinical billing systems manage revenue, controlling expenses, approvals, and payments with the same discipline helps hospitals protect liquidity while receivables move through the revenue cycle.
Book a demo to see how Alaan helps finance teams maintain control alongside complex revenue cycles.
Frequently Asked Questions (FAQs)
1. What is accounts receivable in a hospital setting?
Hospital accounts receivable refers to the money owed to a healthcare facility for services already provided. This includes payments pending from insurance companies, government payers, corporate clients, and patients.
2. Why is hospital accounts receivable management important?
Effective A/R management ensures predictable cash flow, reduces reliance on short-term financing, and supports timely payment of staff, suppliers, and clinical operations.
3. What are common reasons for delayed hospital A/R?
Delays are commonly caused by incorrect patient information, insurance eligibility errors, coding issues, late claim submission, and weak denial follow-up processes.
4. What is a good DSO for hospitals?
Acceptable DSO ranges vary by payer mix and region, but consistently rising DSO is a warning sign. Hospitals typically aim to keep DSO within a controlled, predictable range rather than chasing a single fixed number.
5. How can hospitals improve accounts receivable performance?
Improvements usually come from strengthening front-end processes, increasing clean claim rates, prioritising denial management, using real-time A/R dashboards, and aligning clinical documentation with billing requirements.


.avif)